Problems with drugs and alcohol often co-exist with psychiatric disorders.
Studies have shown that nearly one-third of those with a mental illness have also experienced substance abuse during their lives. Also, over one-third of alcohol abusers and more than half of drug abusers have also had at least one serious mental condition in addition to signs of addictive personality. So if you suspect you or a loved one might be living with an undetected dual diagnosis, gain better understanding of dual diagnosis here and find out why dual diagnosis is more complicated to pinpoint than you might think.
What is dual diagnosis?
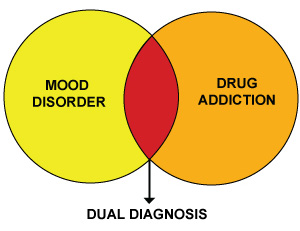
Dual diagnosis is most often defined as a person living with a psychiatric disorder and substance abuse at the same time. Examples could include depression with alcoholism or panic disorder with an addiction to painkillers. Dual diagnosis can also expand to include a psychiatric disorder, such as anxiety, co-existing with a second mental illness, such as personality disorder.
Typically, the initial condition, whether it’s a mental disorder or substance abuse, tends to influence a person’s path to their second condition. Sometimes long-term substance abuse can make way for a psychiatric disorder, while the problems a person encounters from a disorder are often times alleviated with drugs or alcohol which can lead to abuse. For mental health practitioners, this brings into question which condition came first and just how much does one diagnosis thrive from the existence of the other?
Possible origins of dual diagnosis
Researchers have developed theories that help explain how a person may have arrived to dual diagnosis. Below are just a few of those theories:
1. Past-exposure theory – Past-exposure theory suggests that use of non-prescribed psychiatric medications can actually cause mental disorders. Also, new exposure to these medications can increase sensitivity to the effects of drugs and alcohol, making it easier to become addicted and in less time.
2. Self-medication theory – Self-medication theory suggests that those diagnosed with a psychiatric disorder may turn to drugs or alcohol to relieve either the symptoms of their disorder or the negative side effects of their medications.
3. Multiple risk factor theory – Multiple risk factor theory suggests that factors such as poverty, social isolation, traumatic life events, and association with other substance abusers can lead to psychiatric problems and substance abuse.
Challenges diagnosing a dual diagnosis
When a person seeks treatment for more than one condition, it’s important to find a single root cause in order to effectively treat both conditions at the same time. While one diagnosis likely induces the other, it’s not always clear which came first or if an apparent psychiatric disorder is merely a symptom of substance abuse or withdrawal. More often than not, symptoms of perceived disorders disappear after eliminating associated substances. A clear diagnosis will help bring clarity to victim mentality,addiction, or possible mental health issues that can then be resolved.
Assessing and treating dual diagnosis
Before a treatment plan can be devised or the proper program recommended, a person must complete an initial assessment that will determine if dual diagnosis is present or not. Because of the complex correlations between psychiatric symptoms and substance abuse, an official diagnosis of a psychiatric disorder will only be made while a person is clean and sober. Depending on the severity of the addiction, this may sometimes require a stay in a detox treatment center before the dual diagnosis assessment is completed.
If it’s determined that dual diagnosis is present, the most effective program you can enter is one that can provide sufficient treatment for both conditions simultaneously. An integrated approach has proved most effective. Recovery from dual diagnosis can take time and, in fact, it really should in order to properly restore health and maintain an improved quality of life.
Questions about dual diagnosis treatment
Surprisingly, there are few institutions across the U.S. equipped to properly treat dual diagnosis. Alcoholics and drug addicts help for co-existing mental health issues is actually a medical specialty. More commonly found are treatment centers that focus purely on either psychiatric disorders or addiction. You deserve to know your best options for receiving treatment for dual diagnosis. Please contact us below if you have any questions or need recommendations for getting your life back on track.